WELCOME TO CORPORATE FAQ
Here Is The Most Frequently Asked Questions.
Quisque blandit dolor risus, sed dapibus dui facilisis sed. Donec eu porta elit. Aliquam porta sollicitudin ante, ac fermentum orci mattis et. Phasellus ac nibh eleifend, sagittis purus nec, elementum massa.
The new design was a group effort. AAMI/ISO assembled the ISO 80369–3 Project Group
(PG-3). This group is a global representation of clinicians, practice experts, regulators, and industry participants. Through this open forum, any company interested in the ISO 80369 standard was allowed to participate. The PG-3 group identified, validated, and aligned to a global introduction of the new standard connector to systematically replace all prior enteral nutrition connector systems.
The purpose of the new connector is to help reduce the risk of enteral tube feeding misconnections and improve patient safety. The new ISO standard, ISO-80369, has been established for Luer connectors on the nutrition formula end and the patient-access end. There is just one standard nutrition formula connector that will be utilized by all feeding set manufacturers and universally adopted into practice.
Yes, enteral devices, including feeding tubes, administration sets, and enteral syringes are impacted by the initiative. A new enteral-specific ISO standard connector design has been identified and awaits final approval prior to introduction.
New ISO standard connectors have already been implemented and universally adopted
on the nutrition formula end of feeding/administration sets. All enteral device connectors including feeding tubes, administration sets, and medication, flush, and bolus feed syringes are anticipated to comply with the new ISO standard. Enteral-specific syringes will also be required to connect to the new enteral feeding connector for medication, flush, and bolus feed syringes.
What changes are coming to current connectors? And what are the implications of these new standards?
To reduce the frequency of medical tubing misconnections, an international group of clinicians, manufacturers and regulators, such as the FDA, is collaborating with the International Organization of Standardization (ISO) and the Association for the Advancement of Medical Instrumentation (AAMI) to develop ISO 80369 standards. Unique international standard designs will promote better patient safety and help ensure that connectors for unrelated delivery systems are incompatible. The program that is helping introduce the new standards is called the Stay Connected initiative for using safer connectors.
A small-bore connector is a connector with an inner diameter of less than 8.5mm that is used to link or join medical devices, components, and accessories for the purposes of delivering fluids or gases. A Luer connector is a classic type of a small-bore connector used commonly in the healthcare setting. The current universal design of the Luer connector allows for medical tubing misconnections—connections between unrelated delivery systems that have different intended uses (e.g., vascular, enteral, respiratory, epidural, and intrathecal).
While manufacturers are doing everything possible to bring these upcoming changes to the attention of healthcare delivery organizations and plan for an orderly transition in the supply chain, the industry cannot manage the process for healthcare providers. The changes are being brought to the attention of healthcare delivery organizations now to give them adequate time to prepare. They need to put together a multidisciplinary plan to minimize the impact and reduce the risk of unintended consequences.
An introduction plan is under development by industry for each delivery system. The goal in this transition is to ensure that there is no interruption in therapy for the impacted devices and to allow suppliers and providers to work through their existing inventory. Several options are under consideration to aid the delivery of fluids using new connector systems with current/legacy connectors during the transition period. For plans on particular products, contact the supplier. These transitions will be planned carefully and extra care will be necessary to avoid unintended consequences, such as hampering the ability to deliver care.
Color coding is not included in the 80369 standards. The standards will only address connector shape and size. These newly developed engineering controls (forcing functions) make it highly unlikely to bring two unintended connectors together, a development that seems more secure as opposed to relying on memorization of a specific color scheme.
Providers should make sure all personnel within their healthcare organization’s supply chain are fully aware of and prepared for impending changes. Extra effort should be made to effectively manage inventory levels of impacted products with new connectors on the horizon. Manufacturers and other suppliers are aware of the inventory management challenges this transition will cause, and introduction plans are under development for each delivery system. The goal in this transition is to ensure that there is no interruption in therapy for the impacted devices and to allow suppliers and providers to work through their existing inventory. Several options are under consideration to aid the delivery of fluids using new connector systems with current/legacy connectors during the transition period. For plans on particular products, contact your suppliers.
To avoid confusion and reinforce adoption of a common enteral connection, a global industry group representing manufacturers, suppliers, and distributors of enteral nutrition devices has agreed to coordinate a synchronized introduction of the new ISO connectors, which will include:
- Guiding healthcare providers through a careful transition plan
- Developing and executing a coordinated joint communications plan
- Identifying each unique connector with a common name to be used by all suppliers of devices for each respective delivery system
An introduction plan is under development for each delivery system. The goal in this transition is to ensure that there is no interruption in therapy for the impacted devices and allow suppliers and providers to work through their existing inventory. Several options are under consideration to aid the delivery of fluids using new connector systems with current/legacy connectors during the transition period. For plans on particular products, contact your suppliers.
A collaborative approach to transition the market from the current connectors to the new versions is under development and will be communicated through suppliers with advanced warning to prepare for the changes. Information and details about the new design standards and their publication dates, timeline for connector transitions, and educational materials will be available at www.StayConnected2014.org. This website will be the primary source for the latest information on connector changes for each therapeutic group. For details on specific suppliers and their product introductions, please visit their respective websites.
Many organizations believe they have never had a tubing misconnection, but that may not be the case. Many tubing misconnections are discovered before there is harm—these are generally not reported. All organizations are one human error away from a harmful tubing misconnection. All should be concerned about making the care environment safer for patients and clinicians by providing devices that are designed using the principles of human factors engineering.
Depending on the therapeutic group, adopting these new connectors may increase costs to produce the same products. Pricing is at the sole discretion of device manufacturers. Talk to your suppliers to better understand the financial impact, if any, to your organization.
Personnel at healthcare facilities that supply products in any capacity and those that administer or deliver care will be impacted by the connector changes. Personnel responsible for product supply including purchasing/procurement and materials management as well as pharmacists should be brought in early to understand all the implications and actions necessary to prepare for the small-bore connector introduction. Physicians, nurses, nurse practitioners, infusion therapists, and dietitians, among other clinicians, should be informed and trained well in advance of any introductions to avoid any interruption in therapy. Additional functions to consider include healthcare technology management, patient safety, and quality assurance personnel.
As of August 2013, there were no federal mandates for manufacturers or healthcare organizations.
Effective Jan. 11, 2016, a California law (HB 1867) will prohibit general acute care, acute psychiatric, and special hospitals from using an epidural, intravenous, or enteral feeding connector that fits into a connection port other than the type for which it was intended. It is expected that all medical device manufacturers/suppliers will comply with the new California law. In doing so, they will develop modified products that incorporate the new connectors and phase out products with old connectors. The changes and requirements will need to be communicated to clinicians who use the products and to those responsible for product conversions in the organizations.
Also, the FDA issued a letter to manufacturers, healthcare professionals, and hospital purchasing departments in July 2010 that outlines what each group can do to reduce the risk of tubing misconnections. The agency noted they are participating in the development of the ISO standards that will help prevent these misconnections through use of function design and usability testing. The FDA stated it is considering recognizing the ISO standards, and if it does, it will provide guidance to manufacturers regarding the timeline for devices on the market to come into compliance, as well as explain the effect of the standards on new devices.
Healthcare providers are strongly advised to take the following steps as new connectors approach the market:
Aware
- Generate awareness of impending changes across the organizations to all impacted clinicians, administrators, supply chain, health technology management, and other support staff.
- Identify a leader within the organization to stay informed as plans progress and communicate updates to others in the organization early and often.
Prepare
- Form teams to assess existing systems, processes, and protocols that may need to change, focusing on areas of highest risk which have the most immediate need to convert to the new connectors.
- Work with supplier representatives and adopt their product-specific transition plan.
- Train clinicians and materials/inventory management staff for impending changes.
Adopt
- Introduce new connectors into work stream to reduce the risk of tubing misconnections and improve patient safety.
- Remind the organization of the long-term benefits vs. the short-term hassles of transitioning to new connectors.
Measure
- Quantify the organization’s ability to adopt changes.
- Leverage metrics and formal feedback loops to identify ways to improve the organization’s ability to transition for the next phase of connector introductions.
As new connectors become accepted as standards, more detailed information regarding introduction, transition plans, and timing will be provided.
There will be a transition period marked by stages. That approach is under development and will be communicated by manufacturers with advanced warning so that all parties can prepare for the changes in the market. The changes for the new standard connectors will roll out by delivery system. Manufacturers will incorporate the new connectors into their existing offerings where applicable. By working closely with their suppliers, healthcare facilities or providers should be able to convert on a timeline that best suits their needs and those of their patients.
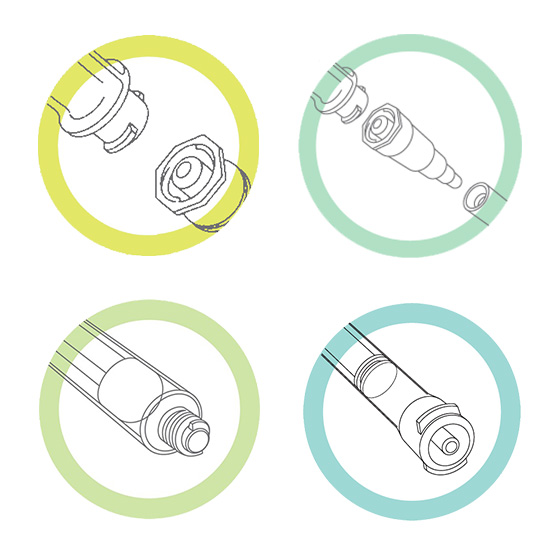
The goal is to develop unique connectors for medical devices for each delivery system so that their inherent design makes it virtually impossible to connect unrelated systems. The new tubing connector designs are based on human factors engineering and computer aided design (CAD) analysis to reduce the likelihood of misconnections. The proposed unique designs for the connectors go through a rigorous process to ensure they connect only to the proper mating connector. Proposed designs are validated through hands-on usability testing to confirm that they meet their intended purpose of preventing the connection of a medical device from one delivery system to a device of another delivery system. Analysis of design drawings and physical force fit testing are used to verify that connectors that are supposed to connect do so securely, while connectors that should not join are physically prevented from doing so.
Manufacturers of breathing systems and driving gases, enteral, limb cuff inflation, and neuraxial devices will need to redesign their products to accept the new connector standards as they are approved. Manufacturers are prepared to launch new connectors with minimal disruption to supply and clinical practice. You should anticipate a phased approach to the launch of new connectors, starting with enteral devices in 2014. Manufacturers are expected to synchronize the introduction of new standard connectors with a transition plan to assist customers’ conversion from existing products in the market.
Unique international standard designs for each high-risk device delivery system will promote better patient safety and help ensure that connectors for unrelated delivery systems are incompatible. Without an international industry design standard for connectors, manufacturers would have to attempt to test against all proprietary designs for different applications to ensure that their connector is incompatible with any other connector on the market. Healthcare organizations would have to purchase multiple systems across the continuum of care—without a standardized mechanism for testing and evaluation to prevent misconnections between them. Such a scenario could create confusion and put patients at higher risk. When the standards are approved, the Luer connector will be maintained only for the intravascular and hypodermic applications. All other delivery systems with small-bore connectors will change to ensure incompatibility with the intravascular Luer connector or each of the other new connectors.
There will be new connector designs for the following device types:
- Respiratory systems and driving gases
- Limb cuff inflation applications
- Enteral feeding
- Neuraxial applications
- When the standards are approved, the existing Luer connector will be maintained only for the intravascular and hypodermic applications. All other delivery systems with Luer connectors will be impacted to ensure non-interconnectability with the intravascular Luer connector, as well as incompatibility with the new connector designs of other delivery systems.
To reduce the frequency of tubing misconnection hazards, an international group of clinicians, manufacturers, and regulators, such as the FDA, is collaborating with the International Organization of Standardization (ISO) and the Association for the Advancement of Medical Instrumentation (AAMI) to develop ISO 80369 standards. The first of these standards, 80369-1, was published in January 2011, and it provides general requirements for connectors for liquids and gases in healthcare applications. It also establishes a framework for testing connectors to ensure non-interconnectability of unrelated delivery systems (e.g., vascular and enteral). International standards for non-Luer-compatible delivery system–specific connections are under development. New connectors are expected to reach the market as early as Q4 2014.
Each additional standard in the series will focus on connectors for a specific clinical application and will be released as it is completed, beginning in 2014. These standards include connectors for breathing systems and driving gases, enteral, limb cuff inflation, neuraxial, and intravascular-hypodermic applications. There will be a phase-in period for product development and implementation guided by the FDA and existing state legislation. California, for example, has been active on this front. (Refer to question 14 for additional information on CA law.)
Alerts and guidance documents have been issued by numerous governmental, accreditation, professional, manufacturing, and healthcare organizations. They include the following:
• Sentinel Event Alert, Issue 36: Tubing misconnections—a persistent and potentially deadly occurrence from The Joint Commission (TJC)
• Case studies, a safety calendar, videos, webinars, and other resources from the US Food and Drug Administration (FDA)
• Clinical recommendations from the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.)
• A letter to surveyors about the need to review hospitals’ prevention policies from the Centers for Medicare & Medicaid Services (CMS)
• Making Healthcare Safer II: An Updated Critical Analysis of the Evidence for Patient Safety Practices from the Agency for Healthcare Research & Quality (AHRQ)
Other organizations have published educational material and practice standards describing methods to reduce tubing misconnections. Healthcare providers have implemented educational programs and protocols, such as tracing all lines back to their origin prior to reconnecting devices, or positioning catheters and tubes that have different purposes on different sides of the patient’s body. Some manufacturers use color coding with their connectors. Others have developed proprietary alternative connectors and product designs that are incompatible with Luer connectors for IV delivery systems, which are frequently involved in misconnections. However, these efforts have not eliminated the problem. A design change and correlating standards would make misconnections between unrelated delivery systems (e.g., vascular, enteral, respiratory, epidural, and intrathecal), medical devices, and accessories highly unlikely. Such design changes should be based on specifications and correlating standards. For more information on how design standards are validated, see question 11.
Liquid formula or medication intended for delivery into the stomach via a feeding tube or nasogastric (NG) tube is connected to an intravenous (IV) line, delivering the formula or medication into the bloodstream. A noninvasive blood pressure inflation tube is connected to an IV line, delivering air under pressure into the bloodstream and causing an air embolism. IV fluids are connected to the inflation cuff on a breathing tube (tracheostomy or endotracheal tube) and deliver a large volume of fluid to a fixed volume device designed to be filled with air (the cuff), resulting in airway obstruction. A tube feeding is connected to a peritoneal dialysis catheter, delivering formula that had been intended for the stomach to the abdominal (peritoneal) cavity.
Unfortunately, the simple and universal design of the Luer connector allows for connection between unrelated delivery systems—that have different intended uses (e.g., vascular, enteral, respiratory, epidural, and intrathecal). As a result, care providers can inadvertently connect wrong systems together, causing fluids (e.g., medications, enteral feedings) or gases (e.g., oxygen) to be delivered through the wrong route. The consequences can be fatal to patients. (REF FDA MEDSUN webcast Nov 2008)
Adoption of international standards for small-bore connectors will ensure compatibility and consistency while reducing the likelihood of misconnections. New connectors will provide:
• Greater ability for different manufacturers’ devices to integrate, while making it
difficult, if not impossible, for unrelated delivery systems to be connected
• Standardized connections across the healthcare settings
• Less likelihood of therapy interruption due to connector incompatibility
or unavailability
A small-bore connector is a connector with an inner diameter of less than 8.5 mm that is used to link or join medical devices, components, and accessories for the purpose of delivering fluids or gases. A Luer connector is a classic type of a small-bore connector used commonly in the healthcare setting
A typical patient could be connected, via tubes or catheters, to several delivery systems to receive medication, nutrients, and fluids. Tubing misconnections—also called Luer misconnections, small-bore misconnections, or wrong route errors—refer to what happens when a tube from the medical device for one delivery system is connected to a system that serves a completely different function—for example, a feeding administration set being connected to a tracheostomy tube. Such errors have resulted in patient injury and deaths, and they are widely recognized as underreported. Misconnections are attributed to the universal design of Luer connectors, which are one of the most commonly used types of small-bore connectors in healthcare. The connectors are parts used to connect the tubing of one medical device to another. However, the simple design and ease of use of the Luer connector allows the tube of the device for one delivery system to be connected to an unrelated system that has a different intended use.



